Left: Measles is transferred through airborne contact (Centers for Disease Control and Prevention)
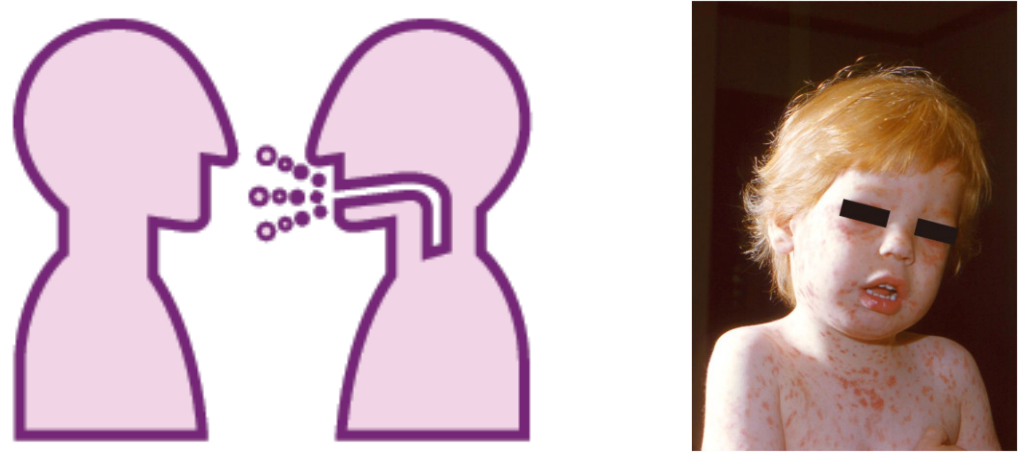
Right: A child with the measles rash (Centers for Disease Control and Prevention’s Public Health Image Library (PHIL))
Measles is a highly contagious viral infection that is spread through airborne contact with respiratory secretions, such as coughing or sneezing. Transmission is possible for up to two hours after an infected person leaves an area, as the virus can linger in the air and on surfaces. Over 90% of individuals who are exposed to measles may become infected after an incubation period of approximately 11–12 days. Initial symptoms include fever, cough, nausea, and conjunctivitis.
Koplik’s spots, tiny white dots that appear in the mouth, may develop 2–3 days after symptom onset and are a distinctive warning sign of measles. Following 2–4 days of initial symptoms, the characteristic rash appears, beginning on the face and spreading downward toward the legs and feet. Fever and systemic symptoms can worsen, with body temperature rising to as high as 40°C (104°F). Measles is contagious from four days before the onset of the rash to four days afterward, and patients are advised to remain in isolation during this period. Individuals who suspect measles infection are encouraged to seek medical attention immediately.
Measles can affect people of all ages but occurs most commonly in unvaccinated children. Infants, pregnant women, and immunocompromised individuals are particularly vulnerable and face the highest risk of severe complications, including pneumonia, encephalitis (swelling of the brain), and death. According to the U.S. Centers for Disease Control and Prevention, the case fatality rate is approximately 1–3 deaths per 1,000 reported cases, most frequently among young children.
History of the Disease
The measles virus is believed to have evolved from the rinderpest virus, which infected cattle and other animals, around the 6th century BCE, adapting over time to infect humans exclusively. Throughout the Middle Ages, measles spread widely across Europe and Asia and was often confused with smallpox, although smallpox was generally more severe and left permanent scarring.
Beginning in the 16th century, European imperial expansion introduced measles to previously unexposed populations worldwide. For example, Spanish colonizers brought measles to Indigenous populations in South America, including the Inca civilization. In the 17th century, measles appeared in North America, with one of the first documented outbreaks occurring in 1829 in what is now the western United States.
In 1954, researchers John Enders and Thomas Chalmers Peebles successfully isolated the measles virus by transmitting it from infected human patients to rhesus monkeys. This discovery marked a major milestone in virology and laid the foundation for vaccine development.
Development of the Vaccine
Early attempts at measles prevention date back to the 18th century. In 1758, physician Francis Home experimented with a rudimentary form of inoculation following a measles outbreak in Edinburgh by exposing healthy children to material from infected individuals. While ineffective by modern standards, this work contributed to early understanding of disease transmission.
Following the isolation of the measles virus in 1954, researchers were able to attenuate, or weaken, the virus through repeated laboratory passages. The first licensed measles vaccine was approved in the United States in 1963. In 1971, Maurice Hilleman, a researcher at Merck & Co., developed a combined measles-mumps-rubella (MMR) vaccine, which remains widely used today. The World Health Organization incorporated the measles vaccine into its Expanded Programme on Immunization in 1974.
Global vaccination campaigns throughout the 1980s and 1990s led to a dramatic decline in measles incidence worldwide. Finland became one of the first countries to achieve sustained elimination of endemic measles transmission in the mid-1990s. Today, measles-related mortality is rare in high-income countries with strong immunization systems. However, in low- and middle-income countries with lower vaccination coverage, measles continues to cause thousands of deaths each year.
Spread and Prevention in China
Left: Cover of a vaccination certificate from Beijing, China (2008)
Right: Vaccination records of an infant from birth to two years old, with measles-containing vaccines highlighted in red
Measles has been present in China since the Middle Ages. National vaccination efforts began in the 1960s, similar to those in many Western countries. The history of measles control in China can be broadly divided into four periods. From 1952 to 1964, measles incidence increased nationwide. After the introduction of a liquid measles vaccine in 1965, case numbers declined, though at varying rates across regions. During this period, vaccination was not mandatory and often required out-of-pocket payment by families.
In 1978, China implemented its Expanded Program for Immunization (EPI), providing measles vaccines free of charge. From 2003 to 2009, large-scale supplementary immunization activities were conducted in 27 of China’s 31 provinces, representing one of the most effective measures in reducing measles transmission.
Under the current national immunization schedule, measles-containing vaccines are administered at 8 months of age, followed by a second dose at 18 months. Vaccines used in the EPI are produced by licensed domestic manufacturers and distributed through China’s public health system. In recent years, measles incidence in China has remained near zero. However, disruptions to routine immunization services and increased vaccine hesitancy during the COVID-19 pandemic resulted in substantial immunity gaps. Global estimates indicate that tens of millions of children missed routine measles vaccinations between 2020 and 2022, raising the risk of future outbreaks through both domestic transmission and imported cases.
Current Epidemic in Canada
Measles cases have risen sharply in Canada in 2025, resulting in the loss of the country’s measles elimination status. As of late 2025, Canada has reported over 5,000 measles cases nationwide. Vaccine hesitancy following the COVID-19 pandemic, along with disruptions to routine childhood immunization programs, have contributed to declining vaccination coverage and increased susceptibility.
Ontario and Alberta have reported the highest numbers of cases. While investigations into some outbreaks remain ongoing, reports indicate that transmission in Ontario initially affected communities with lower vaccination uptake, including certain Mennonite populations. Canada has experienced a higher number of cases than the United States during the same period, despite having a smaller population.
Public health authorities, including provincial health units and the Ontario Ministry of Health, continue to emphasize that measles outbreaks are preventable through vaccination. In Ontario, the first dose of the measles-mumps-rubella (MMR) vaccine is administered at one year of age, followed by a booster dose of the measles-mumps-rubella-varicella (MMRV) vaccine between four and six years of age. Adults who have not previously received the vaccine can also receive MMR through healthcare providers or public health clinics.
Because measles is extremely contagious, vaccination coverage of approximately 95% is required to prevent sustained transmission and achieve herd immunity. Herd immunity occurs when enough individuals are immune to a disease that it can no longer circulate widely, indirectly protecting those who cannot be vaccinated. Maintaining high vaccination coverage is essential to protect vulnerable populations and prevent future outbreaks. Measles is a preventable disease, and widespread vaccination remains the most effective tool to control its spread.
By: Jeanne Lee
Jeanne Lee is a Grade 12 student at Abbey Park High School in Oakville, Ontario. She is passionate about biology and chemistry, and she wishes to pursue a career in healthcare. As a first-generation Chinese immigrant, she is involved in both communities, forging a connection to each aspect of her cultural identity.
